The challenge of microplastic regulation
28. October 2022
Partners in Mission: Nordic Water
27. December 2022Microplastics and human health
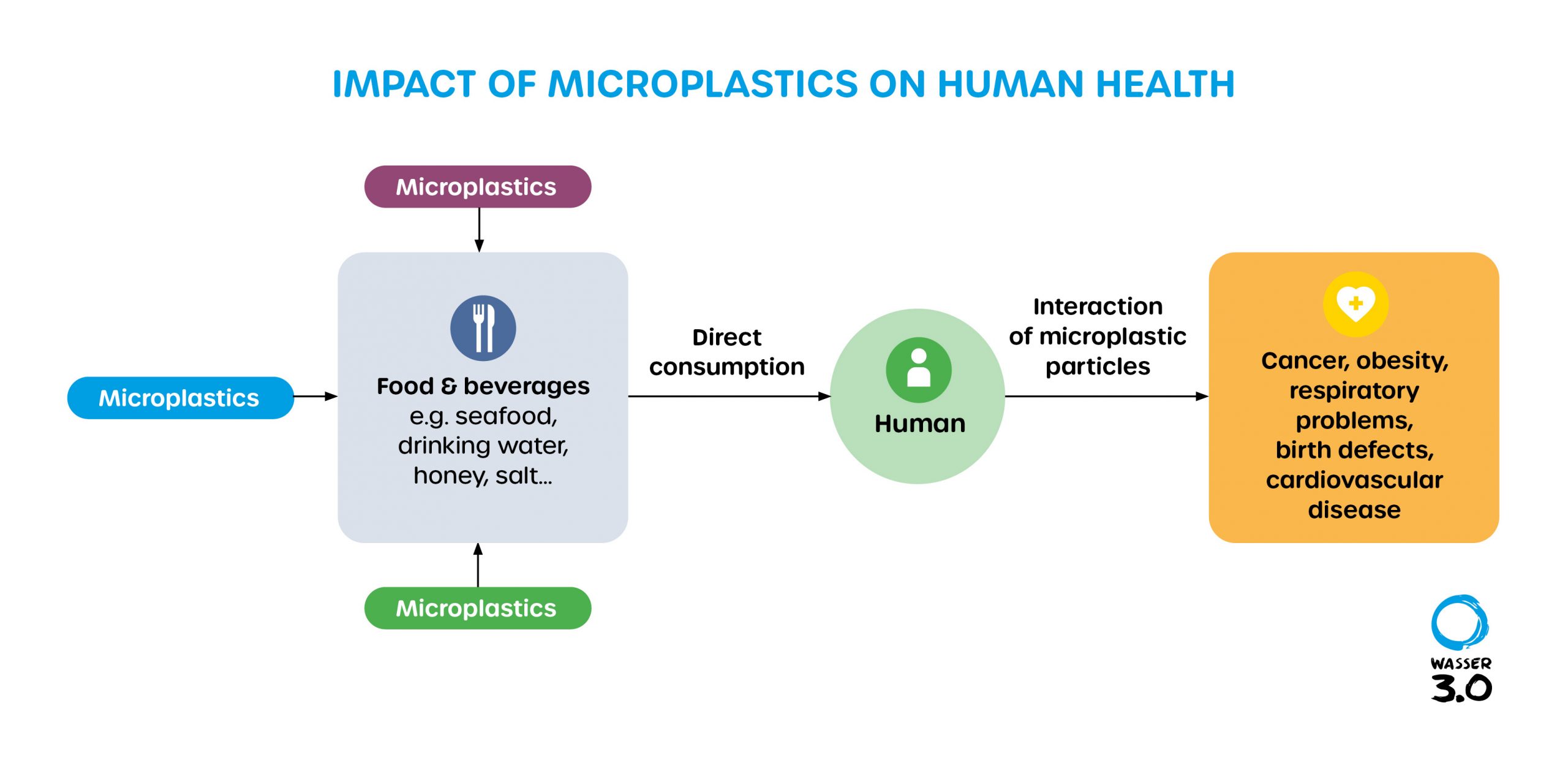
Microplastics have been detected in human blood, deep within the lungs, and in the placenta of unborn babies. Widespread exposure of humans to microplastics is undeniable. But what remains unknown, is what the hazards and toxicological impacts of such exposure are, and what limits need to be implemented for drinking water, food, and the environment. Understanding the impacts of microplastics (< 5 mm) and nano-plastics (< 1 µm) on environmental and human health and the identification of critical thresholds and characterization of hazards, are thus important steps towards effective microplastic management.
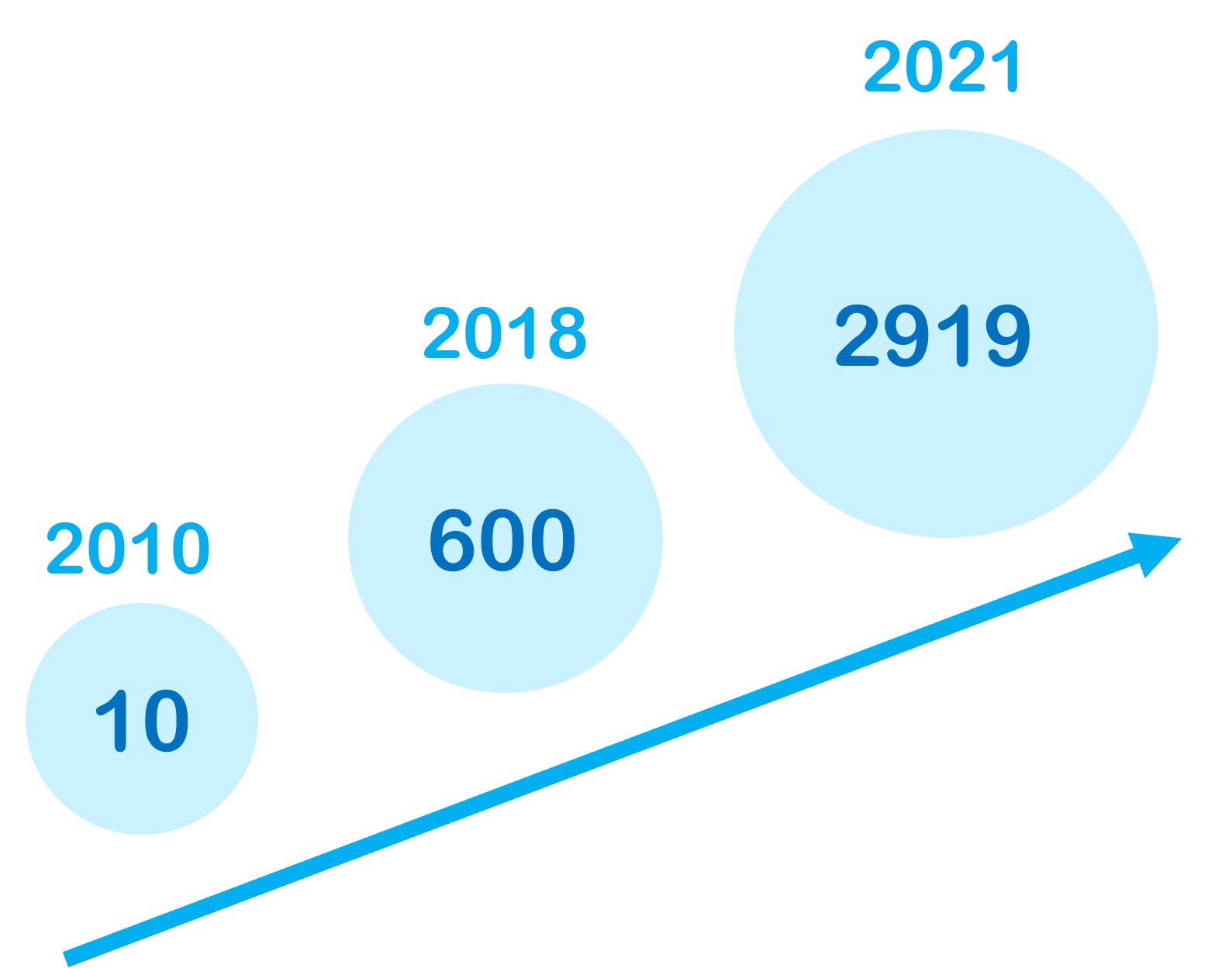
State of microplastic research
A significant amount of research has gone into microplastics in recent years, with just 10 articles per year being published on microplastics in 2010 up to 2919 publications in 2021. But the term that emerges the most within microplastic publications is marine environmental pollution; research on human health impacts is still in its infancy.
Determining the effects of microplastics on humans is a scientific challenge. Validated and standardized analytical methods and reference materials are lacking. Additionally, most studies have been conducted in-vitro (using human-derived cells) using PE and polystyrene beads, even though polyolefins, polyesters, and polyurethanes (PET, PVC, PP, PA) are the most used commercial plastics.
The high variation in particle sizes, shapes, chemical compositions, and distributions/mixtures of microplastics, make it even more difficult to assess their effects on human health. Until now, no studies have investigated environmentally relevant mixtures and real exposure conditions of microplastics and there are to-date no epidemiologic studies that document the connection between microplastics and health impacts within a large groups of people.
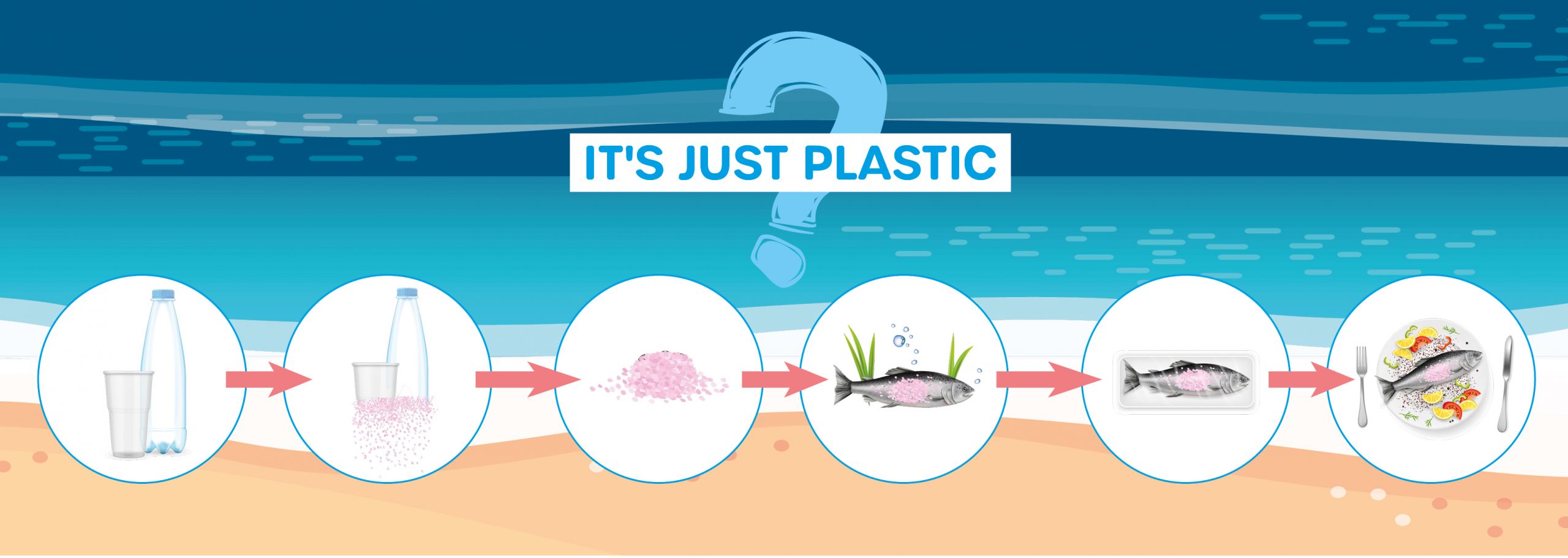
How are nano- and micro-plastics entering the human food chain?
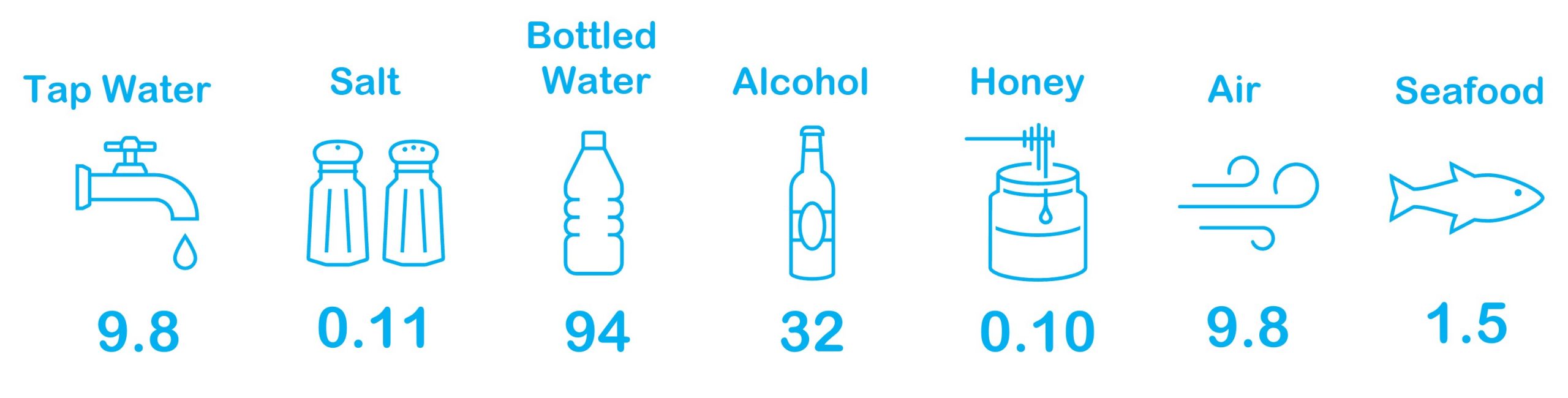
Both nano- and microplastics have been detected in beer, salt, sugar, honey, fish, shrimps, bivalves, and drinking water. Statistics have shown the following concentrations in various sources:
Based on these figures, it has been estimated that humans may consume between 39,000 to 193,000 particles per year, although one study has shown that the ingestion rate may be as high as 30,077,700 microplastics/year when including inhalation. Drinking water has been shown to be one of the primary sources; bottled water typically has higher microplastic count than tap water. One study revealed microplastic levels in bottle water to be as high as > 5E7 microplastics/L. Drinking exclusively bottled water instead of tap water may thus result in the ingestion of an extra 86,000 particles.
The human food chain is a major source of microplastic ingestion, with figures likely even higher, as the level of exposure to microplastics from food packaging and food-contact materials is not yet easily quantifiable.
How has it been quantified so far and what?
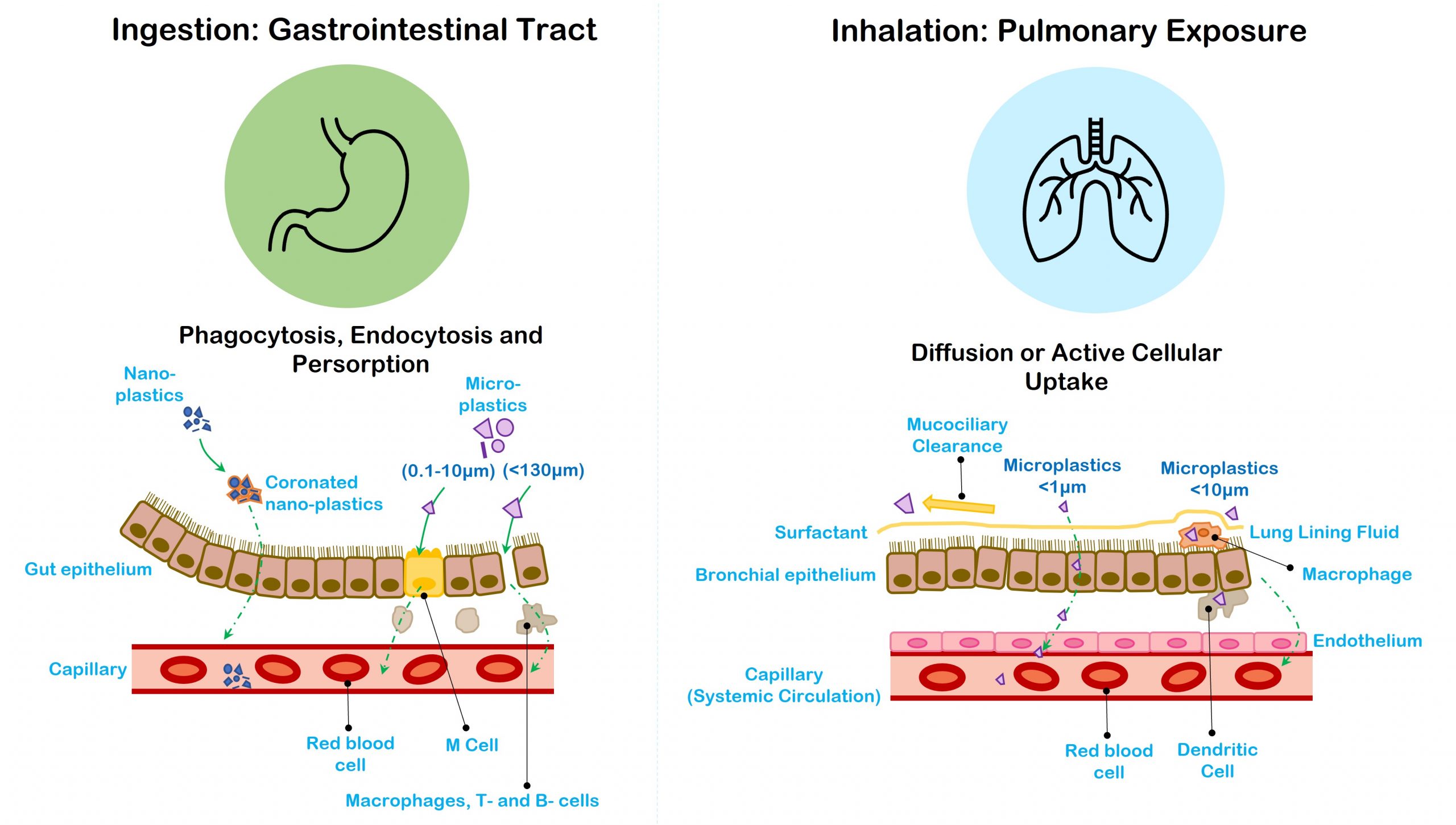
The first step to quantifying the risk of microplastics on human health is to measure the exposure. Humans are frequently exposed to microplastics and uptake into the body is predominantly via ingestion (through food or water), or inhalation. Pulmonary exposure in indoor environments is primarily to fibres from synthetic textiles, while outdoor environments may contain e.g., airborne fertilizer or tire wear particles. The uptake rate and fate of microplastics within the body and organs is assumed to be dependent on not only the size, but also the polymer type.
The size of the particles often determines to which extent they are taken up and distributed by the body. Particles < 10 µm may be inhaled, while those < 1 µm may be taken up by cells. As the particle size decreases, the ability to translocate within the body increases. Generally, only microplastics < 10 µm should be capable of accessing all organs, the placenta, and crossing cell membranes and the blood-brain barrier. Translocation of particles via the systemic circulation into secondary tissues (i.e. the liver, lymph nodes, the spleen, and brain) has been shown for particles between <2.5–5 µm.
What evidence of toxicological effects related to human exposure to microplastics have been determined so far?
The understanding of toxicological risks of microplastics on human health is still in the early stages. This is partly due to a lack of accurate, sensitive, and standardized analytical methods for measuring microplastics in human tissues and levels of exposure (i.e. in air and food) and also due to a lack of information on how environmentally-relevant doses of exposure, along with how the various physical and chemical properties of microplastics, influence the cytotoxicity of microplastics to cells and tissues.
In-vitro studies on human cerebral and epithelial human cell lines have revealed that microplastic exposure may have toxic impacts, such as inflammation, immunosuppression, neurotoxic effects, oxidative stress, autophagic cell death, and apoptosis. These impacts are likely influenced by the type of plastic, level of exposure, the particle shape and size, presence of absorbed pollutants, and the leaching of additives (i.e. bisphenol A) within the plastic material.
Recent studies have also shown that exposure of human lung cells to microplastics may have toxicologic consequences, such as inhibition of cell proliferation and changes in cell morphology, and that an irregular microplastic shape along with microplastic exposure and concentration may be a predictive characteristic for cell death. Environmentally-relevant concentrations of microplastics (10microg/L) have recently been shown to have adverse effects on cell viability and at 20 microg/L cytokine release.
There is concern that further health risks may arise from micro-organisms that grow on microplastic surfaces and from the leaching of hazardous chemical additives. Chemical additives such as bisphenol A (BPA), phthalates, triclosan, bisphenone, organotins and brominated flame retardants (BFR), are all known to negatively impact human health.
Occupational interstitial lung disease has already been long reported among workers in textile industries, particularly for the manufacturing of synthetic textiles, such as nylon, rayon, and polyethylene flock. But the associated adverse effects are thought to be due to physicochemical properties and elevated concentrations of synthetic particles. Thus, health hazards posed by long-term exposures to lower microplastic concentrations, as experienced by the general population, are still to be determined.
Where do we act?
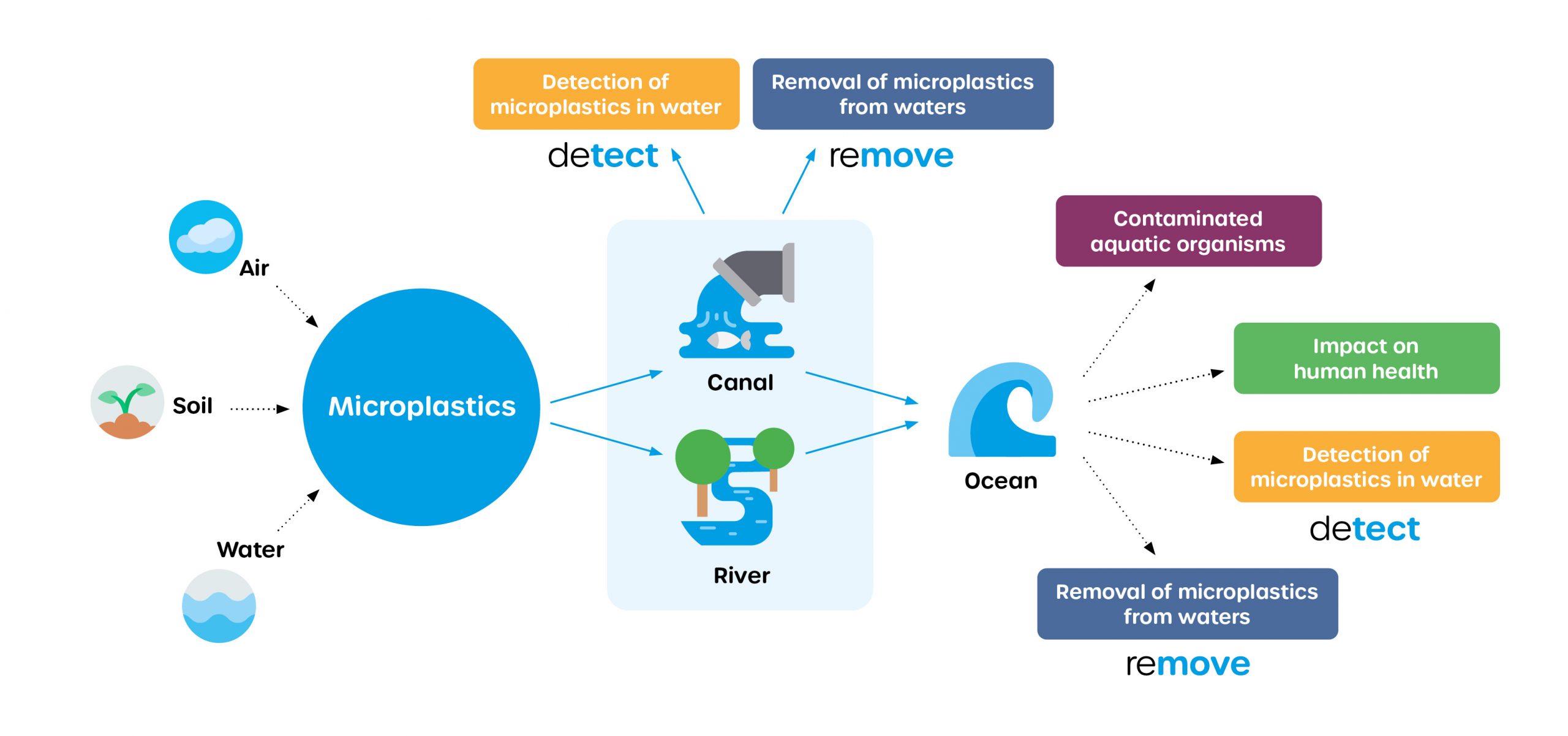
Drinking water is considered to be one of the main sources of human microplastic intake. And effluents from wastewater treatment plants are a major cause of microplastic pollution in freshwater sources of drinking water. The amount of plastic entering the environment and our bodies is increasing and impacting both environmental and human health. Here at Wasser 3.0, we are working to change that. In line with the UN sustainable develop goals, we research and develop innovative concepts and solutions to detect, remove, and reuse microplastics from (waste)water.